The Ominous Octet of Diabetes: The ever-evolving pathophysiology of diabetes mellitus. From the triumvirate to the Ominous Octet (and now the Egregious Eleven). The mechanism of action of various medications in diabetes care will be reviewed.
The Triumvirate
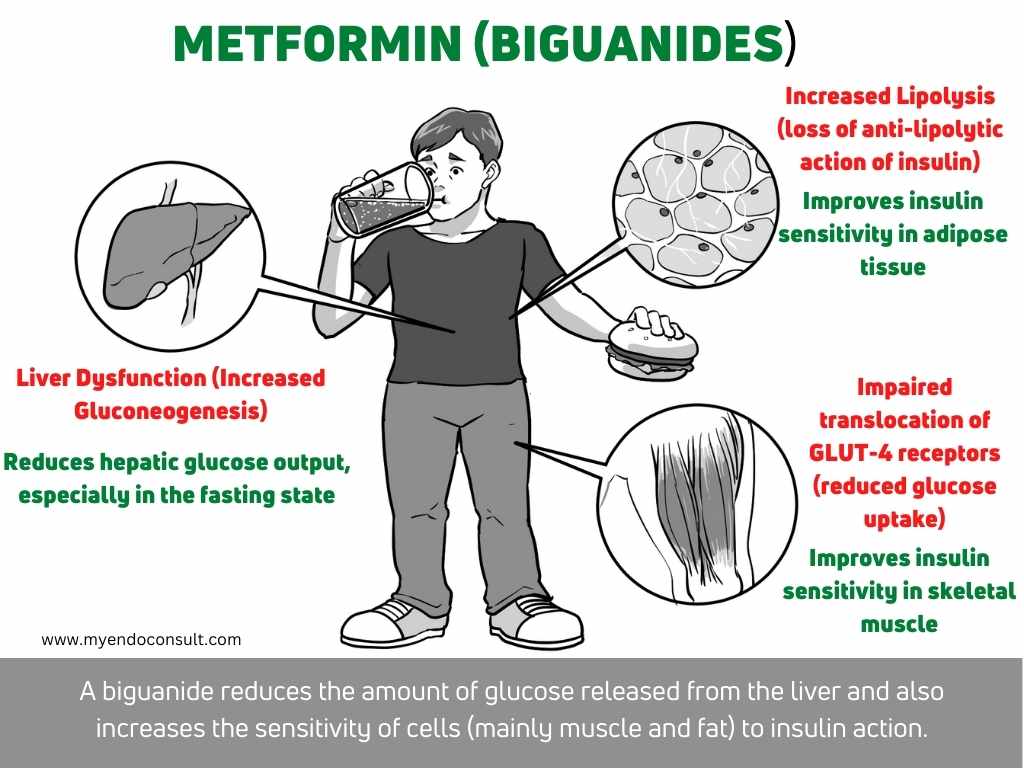
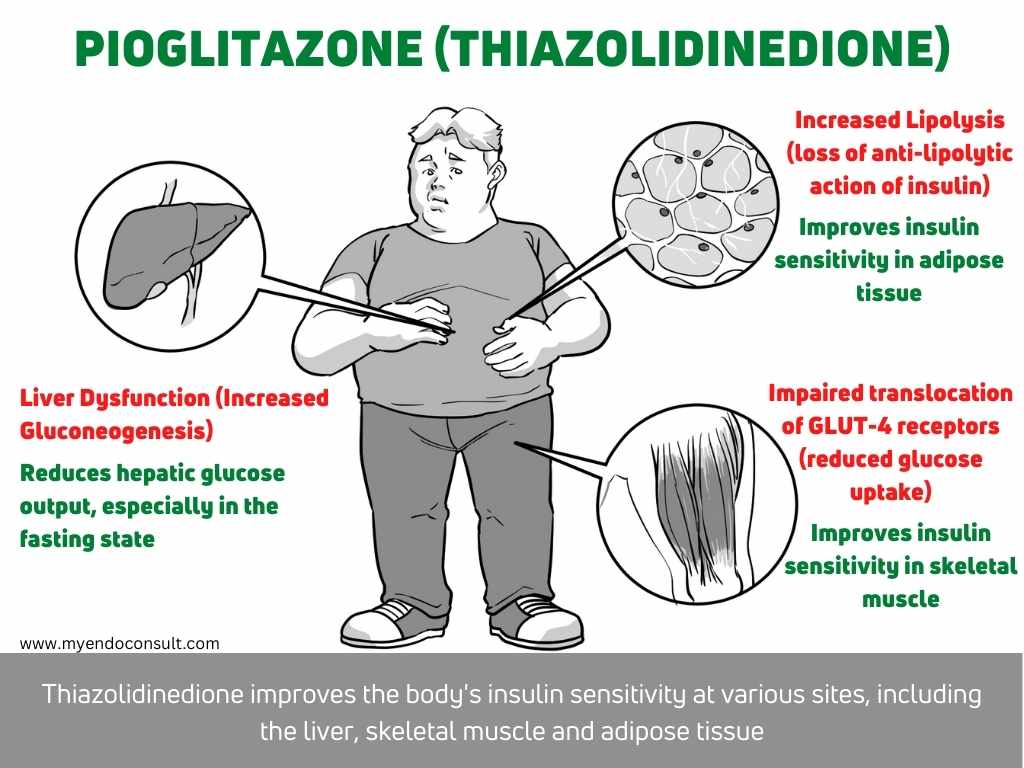
DeFronzo, in 1987, described the Triumvirate of Beta-cell dysfunction, muscle, and hepatic insensitivity to the glucose-lowering effects of insulin[1]. It was postulated that insulin resistance at the liver contributes to fasting hyperglycemia (increased hepatic glucose output) in the early stages of type 2 diabetes mellitus (T2DM).
Beta-cell dysfunction and insulin resistance at the level of skeletal muscle promotes hyperglycemia in the post-absorptive state(decreased glucose uptake). A defect that is demonstrable on the standard oral glucose tolerance test[2]. The triumvirate, which was for a while central to our understanding of T2DM, has since been upstaged by more flowery pathophysiologic mechanisms.
The Dysharmonious Quartet
The Dysharmonious Quartet = The Triumvirate + Adipocyte dysfunction
The diabetic tune was again postulated to include dysregulation at the level of adipocytes[2].
- Adipocytes are resistant to the anti-lipolytic action of insulin. This leads to increased liberation of free fatty acids (FFAs) in the fasting state[3].
- Excess circulating FFAs promotes hepatic gluconeogenesis, hepatic insulin resistance, insulin resistance at the level of the skeletal muscle, and impairs insulin secretion[3].
- Dysfunctional adipocytes produce an excessive amount of pro-inflammatory adipocytokines (tumor necrosis factor, interleukin-6, resistin, and angiotensinogen) at the expense of more insulin-sensitizing adipocytokines such as adiponectin[4].
The Quintessential Quintet
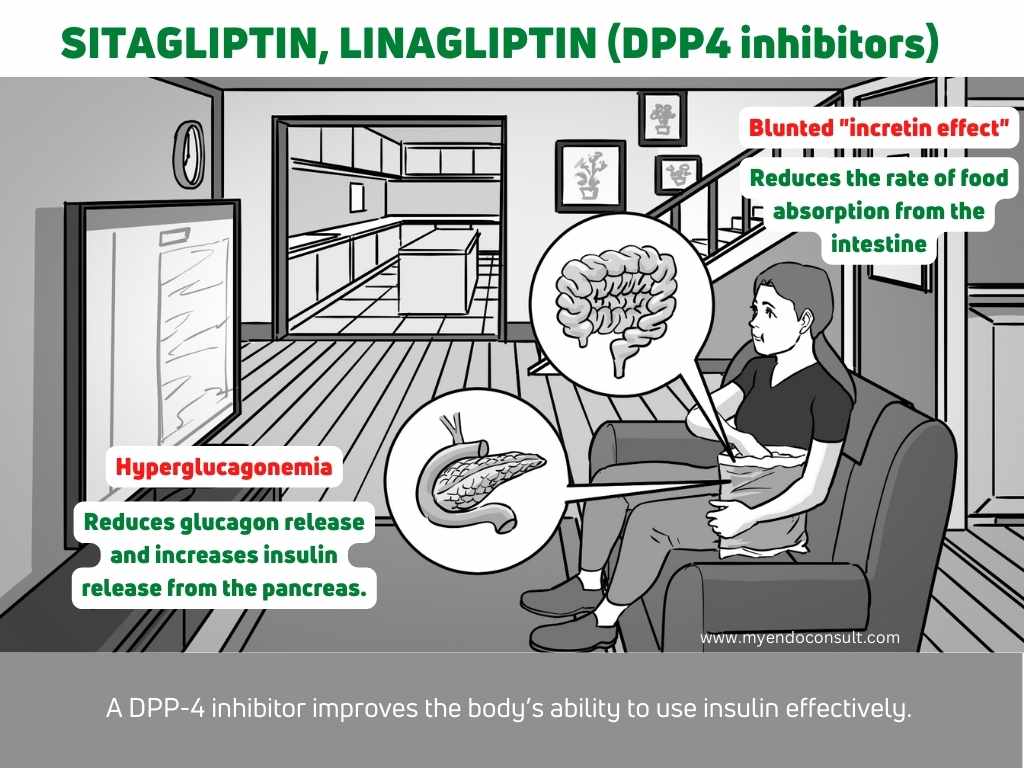
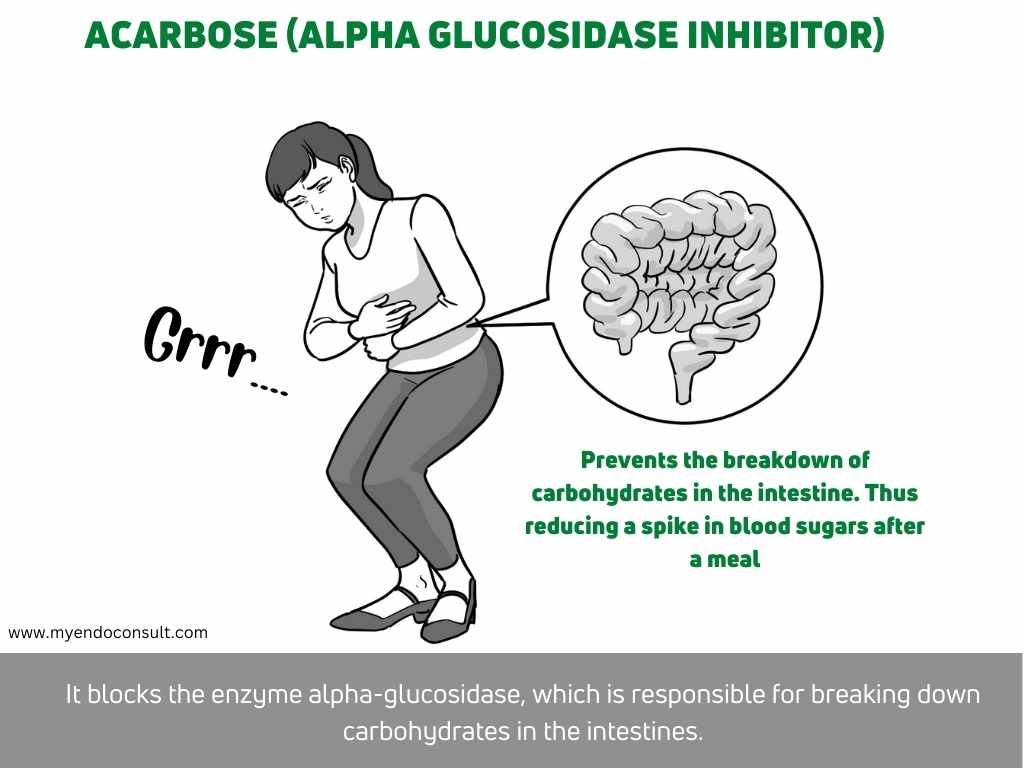
The Quintessential Quintet = Dysharmonious Quartet + Incretin effect (gastrointestinal hormonal dysfunction)
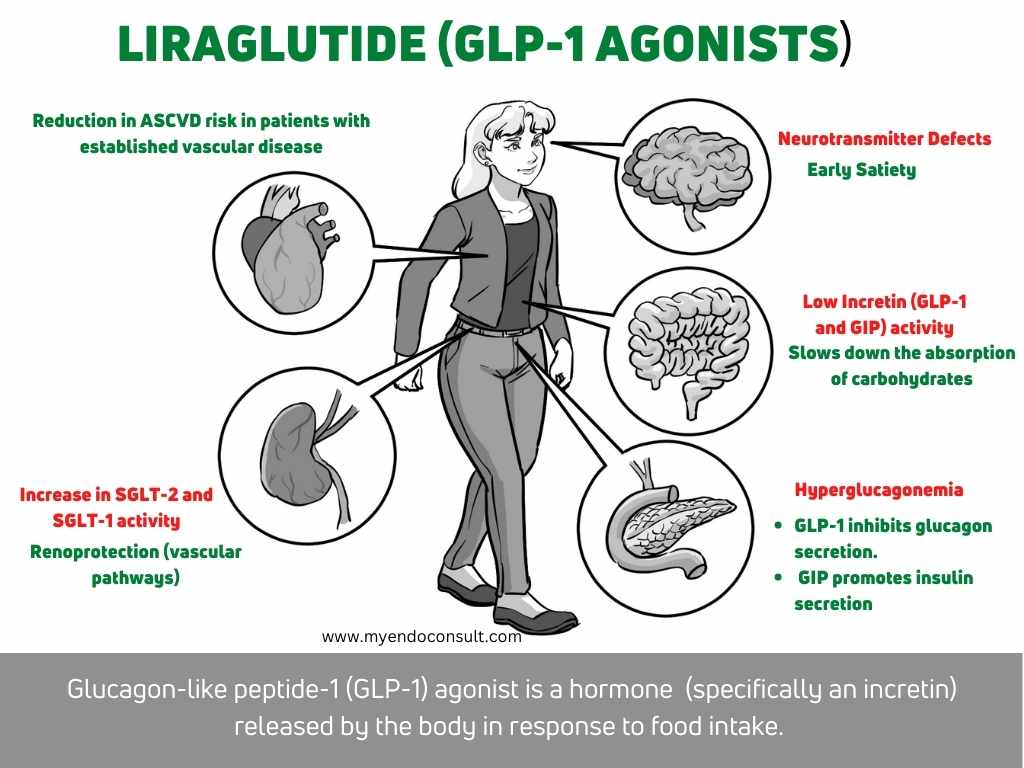
The Quintessential Quintet acknowledges the contribution of the gastrointestinal tract in the pathogenesis of T2DM. What is the incretin effect? – An oral glucose load stimulates a more considerable increase in insulin secretion compared to an intravenous glucose bolus. Indeed, the “incretin effect” occurs as a result of two critical peptide hormones secreted by the digestive tract.
Glucagon-like peptide 1 (GLP-1) secreted by the L-cells of the ileum is woefully inadequate in patients with T2DM. GLP-1 is, therefore, unable to inhibit the secretion of glucagon (a counterregulatory hormone in carbohydrate metabolism). GIP secreted by the proximal small intestine, on the other hand, is increased but is unable to mediate its target organ effects on pancreatic beta cells (i.e., insulin secretion).
- Loss of the glucagon lowering effects of GLP-1 results in hyperglycemia during the post-absorptive state. Unchecked hyperglucagonemia promotes an increase in hepatic glucose output[5].
- GIP, existing in paradoxically high levels, is unable to stimulate increased insulin production[5].
The Setaceous Sextet
The Setaceous Sextet = The Quintessential Quintet + hyperglucagonemia
Pancreatic alpha cell dysfunction leads to significant hyperglucagonemia in the fasting state. This is an essential cause of fasting hyperglycemia[6].
The Septicidal Septet
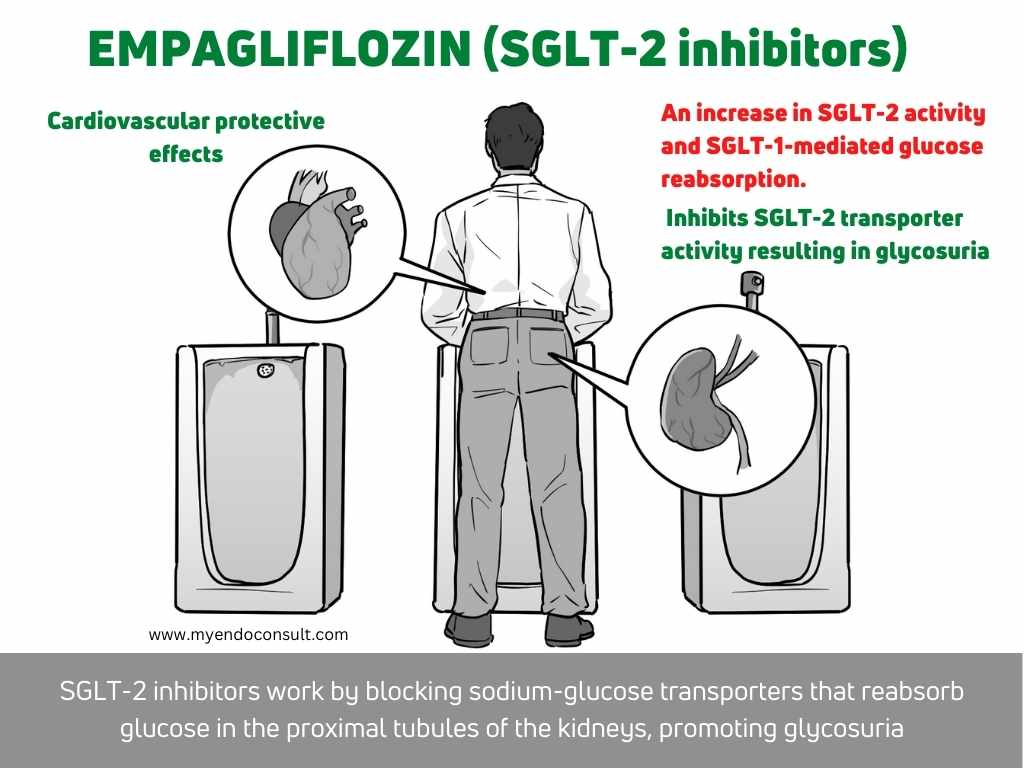
The Septicidal Septet = The Setaceous Sextet + Altered renal glucose handling
SGLT-2 and SGLT-1 transporters present in the proximal tubule of the kidney reabsorbs all of the filtered load of glucose in the proximal tubule. This effectively prevents glucosuria. Interestingly, the upregulation of SGLT2 transporters due to chronic hyperglycemia leads to a maladaptive state in which renal glucose preservation further aggravates diabetes[7].
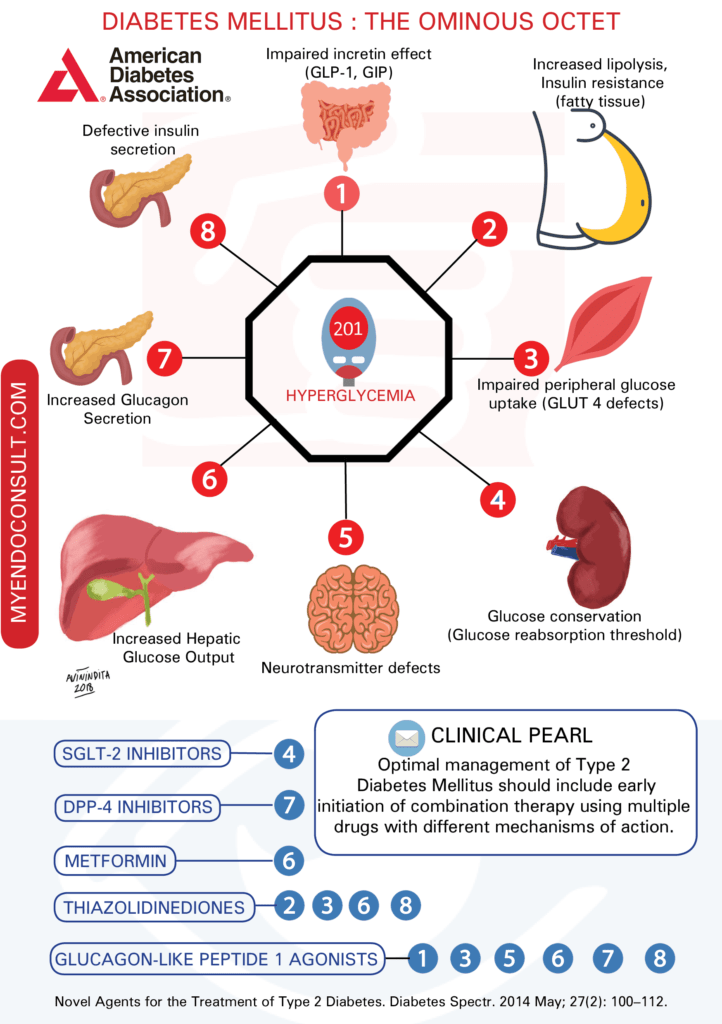
The ominous Octet
The Ominous Octet = The Septicidal Septet + Central Nervous System dysfunction
The Ominous Octet of type 2 diabetes mellitus was proposed by Ralph DeFronzo in 2008. It encompasses 8 pathophysiologic perturbations underlying the onset and persistence of hyperglycemia in type 2 diabetes mellitus. The appetite suppressing effects of insulin are significantly impaired in T2DM. Functional MRI studies have demonstrated dysregulation at key hypothalamic centers responsible for appetite suppression (anorexigenic pathways)[8].

The Egregious Eleven
The Egregious Eleven = The Ominous Octet + Immune dysregulation + Abnormal colonic microbiome + increased rate of glucose absorption (low amylin)
Ominous Octet to Eleven – New mechanisms have been added to the growing list of causes of hyperglycemia. Immune dysregulation and inflammation promote beta-cell dysfunction. Abnormal colonic microbiota is critical in promoting beta-cell dysfunction[9].
Download all of the above infographics for your personal use only. If you require high-quality prints, visit this page. Thanks.
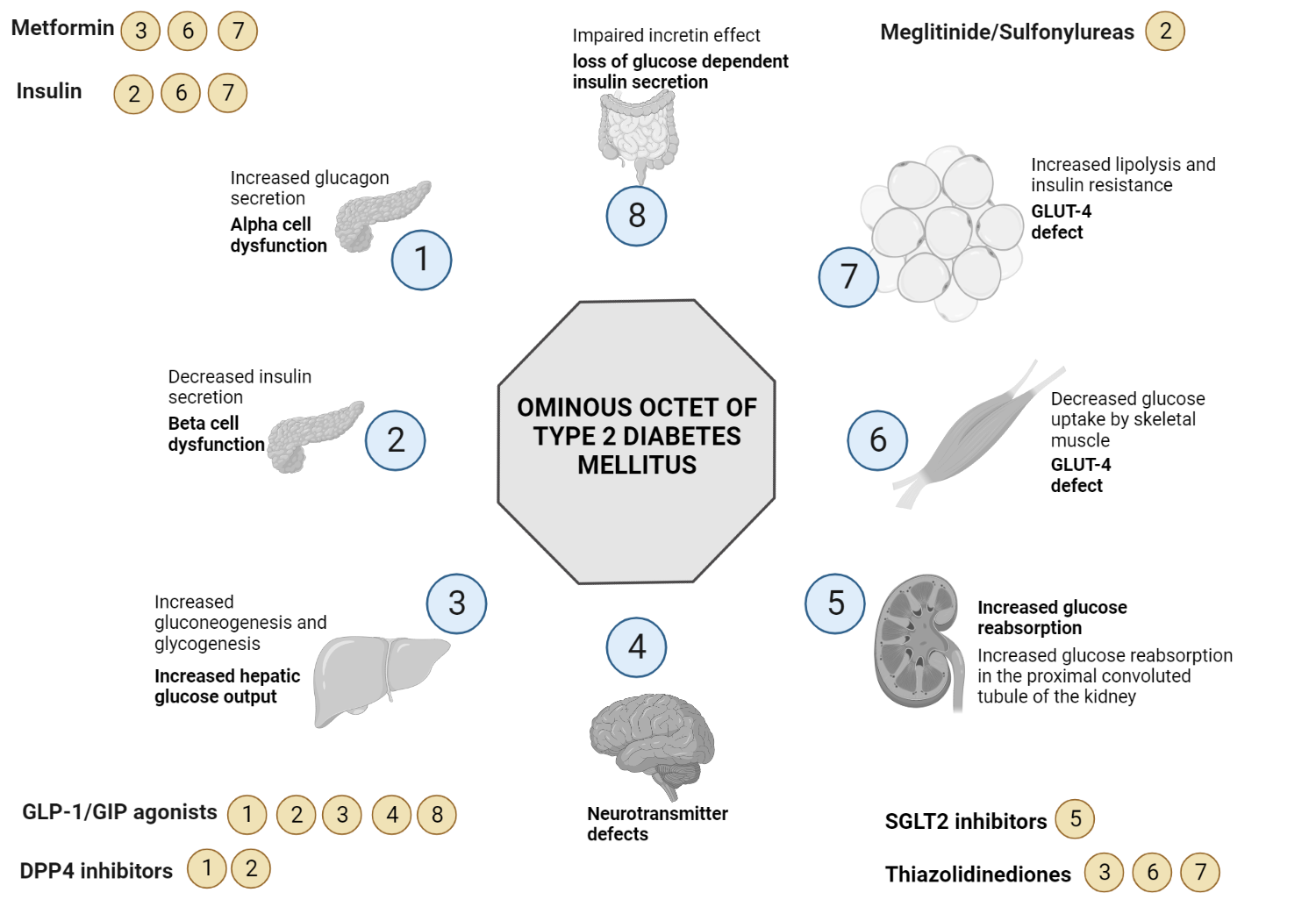
Ominous Octet and Medications for Type 2 Diabetes Mellitus
This infographic summarizes various pathophysiologic abnormalities which result in hyperglycemia (a list of the organs and defects responsible for the ominous octet). Current diabetes medications which address the defects of the ominous octet are also shown.
Dr. Ralph DeFronzo provides a detailed description of the ominous octet and the diabetes triumvirate in this awesome presentation. It is always refreshing to hear the detailed description of a pathophysiology concept by it's proponent. Video credit (@Oscar Moreno via Youtube)
References
- DeFronzo RA (1988) Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 37:667–687
- DeFronzo RA (2009) From the Triumvirate to the Ominous Octet: A New Paradigm for the Treatment of Type 2 Diabetes Mellitus. Diabetes 58:773–795
- Kashyap S, Belfort R, Gastaldelli A, Pratipanawatr T, Berria R, Pratipanawatr W, Bajaj M, Mandarino L, DeFronzo R, Cusi K (2003) A Sustained Increase in Plasma Free Fatty Acids Impairs Insulin Secretion in Nondiabetic Subjects Genetically Predisposed to Develop Type 2 Diabetes. Diabetes 52:2461–2474
- DeFronzo RA, Triplitt CL, Abdul-Ghani M, Cersosimo E (2014) Novel Agents for the Treatment of Type 2 Diabetes. Diabetes Spectr Publ Am Diabetes Assoc 27:100–112
- Meier JJ, Nauck MA (2006) Incretins and the development of type 2 diabetes. Curr Diab Rep 6:194–201
- Baron AD, Schaeffer L, Shragg P, Kolterman OG (1987) Role of Hyperglucagonemia in Maintenance of Increased Rates of Hepatic Glucose Output in Type II Diabetics. Diabetes 36:274–283
- Abdul-Ghani M, DeFronzo R (2008) Inhibition of Renal Glucose Reabsorption: A Novel Strategy for Achieving Glucose Control in Type 2 Diabetes Mellitus. Endocr Pract 14:782–790
- Matsuda M, Liu Y, Mahankali S, Pu Y, Mahankali A, Wang J, DeFronzo RA, Fox PT, Gao JH (1999) Altered hypothalamic function in response to glucose ingestion in obese humans. Diabetes 48:1801–1806
- Schwartz SS, Epstein S, Corkey BE, Grant SFA, Gavin JR, Aguilar RB (2016) The Time Is Right for a New Classification System for Diabetes: Rationale and Implications of the β-Cell–Centric Classification Schema. Diabetes Care 39:179–186
Kindly Let Us Know If This Was helpful? Thank You!



Glad it was helpful.
Excellent very helpful