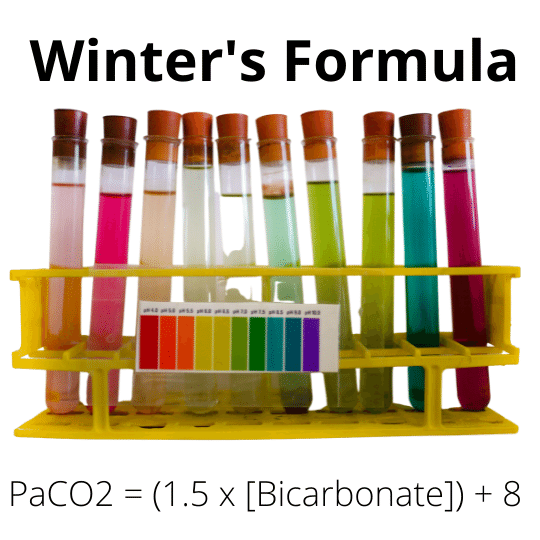
Winter Formula is a useful approach to predicting the partial pressure of carbon dioxide (PaCO2) in patients with metabolic acidosis. The predicted PaCO2 is then compared to the actual value of PaCO2 measured via an arterial blood gas. It is a useful measure for evaluating if respiratory compensation for metabolic acidosis is sufficient. The predicted PaCO2 = 1.5 x [Bicarbonate] + 8. Bicarbonate is in mEq/L while PaCO2 is in mmHg.
A simplified approach (acid-base disorders)
when evaluating acid-base disorders, it is important to explain that the primary disorder has either a state of acidosis or alkalosis. More importantly, due to compensatory mechanisms, patients might have a normal pH. As such, normal pH does not exclude the presence of a primary acid-base disorder. Also, patients might sometimes have double acid-base disorders or, on rare occasions, triple-base disorders.
The Winters formula is helpful in assessing respiratory compensatory mechanisms to an underlying cause of metabolic acidosis. A simplified approach to assessing metabolic acidosis will be reviewed next.
Evaluation of serum pH (step one)
The first step in evaluating an acid-base disorder is to review the serum pH. In simple terms, normal serum pH lies within a very narrow range between 7.35 and 7.45 on the pH scale. For values greater than 7.45, this will represent an alkalotic state primarily. Conversely, a pH less than 7.35 represents a state of acidosis (acidemia).
It is worth noting that the human body does not overcorrect a primary disorder unless there is a concomitant secondary disorder (also known as a mixed acid-base disorder); as such, pH is certainly helpful during the initial assessment for an acid-base disorder.
Assessment of the primary disorder (respiratory or metabolic)
After determining whether the patient is in an acidotic or alkalotic state, we will need to assess whether this is due to a respiratory or metabolic condition. A simple rule of thumb is that normal serum bicarbonate is about 24 mEq per deciliter (+/-2) while a normal serum PCO2 is 40 mmHg (+/-5).
Evaluate respiratory compensation
In patients with metabolic acidosis, the body’s compensatory mechanisms to correct acidosis need to be evaluated. The respiratory system plays a pivotal role in correcting metabolic acidosis.
To offset a decline in serum pH, hyperventilation occurs in an attempt to lower the partial pressure of carbon dioxide. A subset of patients will be unable to mount appropriate respiratory compensation leading to an additional disparity course of acidosis.
Winter’s formula serves as a useful means to evaluate respiratory compensation. By comparing the patient’s actual PaCO2 to the expected value of PaCO2, the presence or absence of appropriate respiratory compensation will be determined.
Winter’s formula (predicted or calculated value of PaCO2) = 1.5 x [Bicarbonate] + 8
Interpretation of Winters formula: if the measured partial pressure of carbon dioxide is not close to what is predicted by winter’s formula, then a second disorder coexists. For example, if PCO2 is less than the predicted value, secondary respiratory alkalosis is present. Conversely, concomitant respiratory acidosis is present if PCO2 is greater than the predicted value.
Calculate the Anion Gap
Formula for the anion gap = [Na+] – ([HCO3] + [Cl-])
A normal anion gap is 12 (+ or -2). In patients with hypoalbuminemia, anion gap should be corrected for serum albumin. In effect, for every 1g/dL decline in serum albumin from the normal value of 4 g/dL, +2.5 should be added to the estimated anion gap.
The differential diagnosis for a high anion gap metabolic acidosis (HAGMA) , remembered using the memory device “MUDPILES)
M: methanol
U: uremia
D: DKA*/Drugs (e.g., metformin or topiramate)
P: phosphate/paraldehyde
I: ischemia/isoniazid (rare)/iron (rare)
L: lactate
E: ethylene glycol
S: starvation/salicylates
Normal anion gap metabolic acidosis occurs when there is an increase in serum chloride (an anion). This measured anion does not cause an increase in the estimated or calculated anion gap.
This has led to some authors referring to this with a somewhat erroneous term called non-anion gap metabolic acidosis. A more accurately descriptive term for this should be a normal anion gap metabolic acidosis.
A simple memory device for recalling the differential diagnosis of normal anion gap metabolic acidosis is “DURHAM.”
D: diarrhea
U: ureteral diversion
R: renal tubular acidosis
H: hyperalimentation
A: Addison’s disease/acetazolamide/ammonium chloride
M: miscellaneous (chloridorrhea, amphotericin B, toluene*, others)
The urine anion gap needs to be estimated to differentiate between renal tubular acidosis and other causes of normal anion gap and metabolic acidosis.
Patients may, on occasions, have low anion gap metabolic acidosis. These causes of low anion gap metabolic acidosis are not associated with deleterious outcomes.
For example, albumin is a negatively charged protein (anion); as such, hypoalbuminemia leads to a decrease in the measured anion gap. Multiple myeloma in bromide ingestion is another cause of low anion gap metabolic acidosis.
This can also be remembered using the memory device or mnemonic known as “BAM”:
B:Bromism (ingestion of bromo seltzer)
A:Albumin (low albumin)
M:Multiple myeloma
Coexistence of elevated anion gap and normal anion gap metabolic acidosis
it is worthy to note that an elevated anion gap metabolic acidosis and normal anion gap metabolic acidosis may coexist in the same clinical setting (mixed acid-base disorder). A simple rule of thumb to evaluate this is based on the assumption that for a pure elevated anion gap metabolic acidosis, serum bicarbonate is expected to decline by the scene amount that the anion gap increases.
This is sometimes referred to as the Delta Delta equation (Delta gap). For example, if a patient with metabolic acidosis has an anion gap that is increased by a magnitude of 10 (from baseline), serum bicarbonate would be expected to have declined by a commensurate value of 10 (from baseline). In a scenario where serum bicarbonate declines more significantly than the increase in anion gap, an additional metabolic acidosis is present.
Indeed, this additional cause of metabolic acidosis is causing a significant decline in serum bicarbonate but not directly affecting the anion gap to the same degree. This should clue one into the diagnosis of concomitant normal anion gap metabolic acidosis.
References
Albert MS, Dell RB, Winters RW. Quantitative displacement of acid-base equilibrium in metabolic acidosis. Ann Intern Med. 1967 Feb;66(2):312-22.
Kindly Let Us Know If This Was helpful? Thank You!


