Syndrome of inappropriate ADH secretion (SIADH) is a syndrome characterized by the excessive output of antidiuretic hormone (ADH).
The most common features of SIADH include hyponatremia (low blood sodium levels) and hypoosmolarity (low blood osmotic pressure). In severe cases, SIADH can also lead to seizures, coma, and death. Treatment for SIADH typically involves correcting the underlying cause of the condition and managing the symptoms. In some cases, this may require medication or surgery.
ADH is produced by the posterior pituitary gland in response to various stimuli, and it helps to regulate water balance in the body. When there is too much ADH in the bloodstream, it can lead to SIADH.
Pathophysiology of SIADH
The pathophysiology of SIADH is complex and may involve different mechanisms. The antidiuretic hormone (ADH) is responsible for water reabsorption in the kidney by stimulating the insertion of water channels (aquaporins) in the cell membranes of the collecting ducts. AVP is a non-osmotic ADH released from the pituitary in response to different stimuli, like pain, dehydration, or stress.
When AVP is released in excess, it can lead to SIADH by increasing water reabsorption in the kidney and consequently reducing urine output. SIADH can also be caused by medications or diseases that cause an increase in AVP release or that reduce urine output. In addition, genetic factors may also play a role in the pathophysiology of SIADH.
The most common malignancy associated with SIADH is small cell lung cancer, but other malignancies such as thymoma, ovarian cancer, and Hodgkin’s lymphoma have also been reported.
Medications associated with SIADH include SSRIs, anticonvulsants, cyclophosphamide, vincristine, and some antibiotics. Infections that have been linked to SIADH include pneumonia and meningitis.
AVP, or Antidiuretic hormone, is a hormone that helps the body to conserve water. It does this by causing the kidney to reabsorb water from the urine and return it to circulation. AVP is produced in the pituitary gland and released in response to increased blood concentration or dehydration. AVP binds to V2 receptors on the basolateral membrane of cells in the distal tubule and collecting duct of the kidney.
This activates a second messenger cascade that leads to the insertion of AQP2 channels into the apical membrane. AQP2 channels allow water to move from the tubule lumen into cells, where it is reabsorbed into circulation. Aquaporins are water-channel proteins that facilitate the movement of water across cell membranes. In addition to AQP2, there are several other aquaporins that play important roles in renal water balance, including AQP3 and AQP4 (read more).
Clinical Features of SIADH
Bartter and Schwartz first described SIADH in 1956, and it is now considered the most common cause of hyponatremia.
The key diagnostic criteria for SIADH are hypoosmolality, euvolemia, and the absence of other known causes of hyponatremia, such as adrenal or thyroid insufficiency.
Investigations
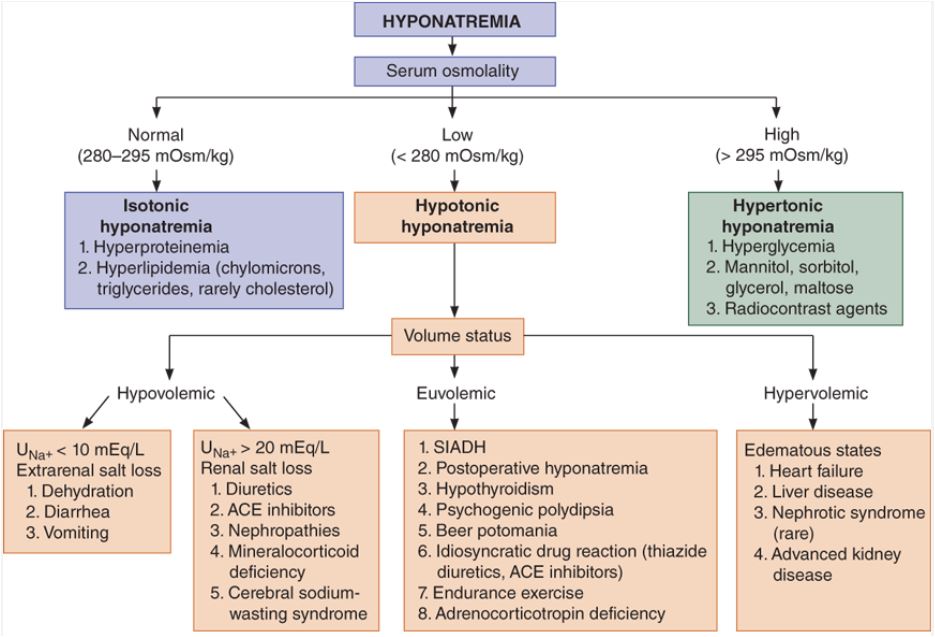
Algorithm for evaluating hyponatremia
Diagnostic criteria for SIADH
- True plasma hypoosmolality
- Urine concentration inappropriate for plasma osmolality (.i.e Urine Osm >100 mOsm/kg H2O)
- Clinical euvolemia in the absence of diuretic therapy
- No evidence of renal sodium conservation (Urine sodium >30 mmol/L)
- Normal thyroid, adrenal and renal function.
Treatment of SIADH
Treatment of malignancy-associated SIADH usually involves the treatment of the underlying malignancy. Medication-associated SIADH typically resolves when the offending medication is discontinued. Treatment of infection-related SIADH generally includes the use of antibiotics and supportive care.
The acute management of hyponatremia includes the infusion of hypertonic saline and the use of vaptans (conivaptan and tolvaptan). Long-term treatment of hyponatremia includes fluid restriction, demeclocycline, furosemide + salt, mineralocorticoids, urea, or vaptans.
A formula for calculating the correction rate for sodium in patients with hyponatremia, using hypertonic saline. This is the protocol for use of hypertonic saline.
- Choose the desired correction rate of plasma sodium. An example is 1.0 mEq/L/h
- Obtain the patient’s body weight in kilograms
- Multiply the estimated body weight x desired correction rate to obtain the infusion rate of hypertonic saline (ml per hour).
- For a 70kg man with a desired correction rate of 1.0 mEq/L/h, the infusion rate for 3% NaCl will be 70ml per hour.
Fluid restriction
Restrict all intake that is consumed via drinking and not just plain water. The goal is to restrict fluid intake to 500ml/day below the previous 24-hour urine volume or output.
Predictors of likely failure of fluid restriction include a high urine osmolality of >500mOsm/kg of H20, the sum of urine sodium and potassium exceeding serum sodium concentration, 24 hour urine volume <1500ml/day.
Estimating the level of fluid restriction in hyponatremia requires the use of the Furst Equation. This is sometimes called the urine to plasma electrolyte ratio. Divide the sum of urine sodium and potassium by plasma sodium to determine the ratio. Refer to the table below.
| Urine/Plasma electrolyte ratio | Recommended fluid consumption |
| > 1.0 | 0 mL |
| 0.5-1.0 | Up to 500 mL |
| <0.5 | Up to 1L |
Furosemide and Salt supplements
Furosemide is a diuretic that helps to remove excess fluid from the body by increasing urine output. In SIADH, the body retains too much water and electrolytes, resulting in symptoms such as fatigue, nausea, and muscle cramps. SIADH can be treated with furosemide, but it is important to monitor sodium levels closely.
Furosemide can cause the body to excrete too much sodium, leading to dehydration. To prevent this, patients may be advised to take sodium chloride supplements or to increase their intake of salty foods. With proper treatment, SIADH can be managed effectively.
Demeclocycline
Demeclocycline is a tetracycline derivative that has been used for the treatment of SIADH. It works by inhibiting the ADH-mediated concentrating ability of the kidney, which results in an increase in urinary output and a decrease in serum osmolality.
Although it is effective at treating SIADH, demeclocycline has a number of side effects, including nephrogenic diabetes insipidus and ototoxicity. In addition, it is not approved by the FDA for use in SIADH patients. As such, it should only be used as a last resort when other treatments have failed.
Vaptans
Treatment for SIADH typically involves the use of vaptans, which are medications that block the action of ADH.
References
Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2008 Jul;3(4):1175-84.
Zenenberg RD, Carluccio AL, Merlin MA. Hyponatremia: evaluation and management. Hosp Pract (1995). 2010 Feb;38(1):89-96.
Images(s) Courtesy
M.A Papadakis et al, current medical diagnosis and treatment 2017, 56th edition (Hyponatremia Algorithm).
Kindly Let Us Know If This Was helpful? Thank You!


