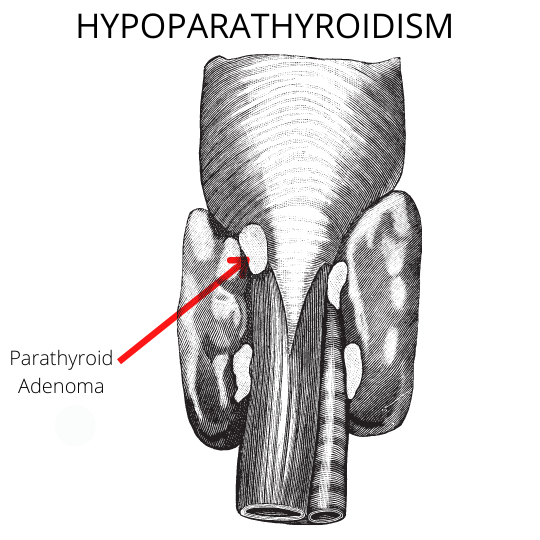
Hypoparathyroidism is a condition in which the parathyroid glands are underactive and do not produce enough parathyroid hormone (PTH). This hormone regulates calcium levels in the blood and is essential for bone health. Without enough PTH, blood calcium levels drop, leading to symptoms such as muscle cramps, fatigue, and anxiety. Hypoparathyroidism can be caused by surgery to remove the parathyroid glands, radiation therapy, or certain medications. In some cases, the cause is unknown.
Treatment Options
Calcium and calcitriol supplementation remains the mainstay of treatment in patients with hypoparathyroidism
- Calcium at doses of 1–9 g/d and calcitriol 0.25–2 μg per day in divided doses
- Calcitriol is preferred over alfacalcidol because of the latter’s shorter duration of action which enables rapid reversal in the event of inadvertent iatrogenic hypercalcemia
- Thiazides reduce the risk of urolithiasis by reducing calciuresis (calcium excretion). This reflexively assists in the amelioration of hypocalcemia.
- For patients with hypovitaminosis D, vitamin D repletion with cholecalciferol may decrease the requirement for calcitriol and calcium.
- Phosphate binders like calcium carbonate are reasonable in patients with significant hyperphosphatemia. This helps in normalizing the calcium phosphate solubility product
Monitoring during treatment
The aims of treatment in a patient with hypoparathyroidism are the resolution of hypocalcemia symptoms and the prevention of long-term complications.
Biochemical targets
- Serum calcium in the low–normal range
- Serum phosphate in the high–normal range
- Maintain a calcium phosphate solubility product <55 mg 2 /dl 2
- Urinary calcium excretion on 24-hour urine collection should be <300 mg/day
Reasons for above targets
- Attempts to raise serum calcium to the normal range with high doses of calcium supplements might exacerbate hypercalciuria and promote urolithiasis. Remember, PTH is required for urinary calcium conservation. The profoundly impaired role of PTH action accounts for this.
- If 24-hr urinary calcium excretion exceeds 250 mg, patients should be started on a thiazide diuretic and low salt diet.
- serum calcium, phosphate, creatinine, and urinary calcium should be measured closely after initiating treatment and less frequently after stabilization.
- Serial serum PTH monitoring is not required.
Indications for treatment with calcitriol
Calcitriol {1,25(OH)2D 3 } is synthesized from 25(OH)D3 by the enzyme 1α-hydroxylase (proximal convoluted tubule of kidney)
- Chronic kidney disease
- Hypoparathyroidism
- Pseudohypoparathyroidism
- Hypophosphatemic osteomalacia
- Renal tubular acidosis
- Hungry Bone Syndrome after parathyroidectomy for primary hyperparathyroidism.
- Postoperative hypocalcemia after parathyroidectomy
- Vitamin D-dependent rickets, type 1 (inactivating mutations
of 1α-hydroxylase), and type 2 (vitamin D receptor defects)
Role of Rh-PTH(1-84) in hypoparathyroidism
Recombinant human PTH (1-84), (Natpara), is indicated for the treatment of calcium and vitamin D metabolite refractory primary hypoparathyroidism. Natpara was unfortunately withdrawn temporarily from the market in September 2019 after rubber particulate material was found in the administered medication. The manufacturer is now working with the FDA to get this medication reapproved for the US commercial market. As at March 2022, the drug is available in the US under a special use program limited previously enrolled patients.
- Osteosarcoma risk in rats. The osteosarcoma risk is dependent on the dose and duration of therapy)
- All patients should be enrolled in the NATPARA Risk evaluation and mitigation strategy (REMS) program
- rhPTH (1-84) 50mcg administered subcutaneously daily into the alternate thigh.
- The dose of oral calcium or calcitriol should be decreased by 50% at the time of initiating rhPTH(1-84)
- Monitor serum calcium every 3-7days with adjustments of calcium/calcitriol until stabilization of serum calcium.
- Dose titration in increments of 25 mcg every four weeks up to a maximum daily dose of 100 mcg.
- The goal is to achieve serum calcium of 8 mg/dL.
Contraindications to rhPTH (1-84)
- Paget’s disease of bone (PDB)
- Unexplained elevations of alkaline phosphatase
- Pediatric and young adult patients with open epiphyses
- Hereditary disorders predisposed to osteosarcoma
- Prior history of beam or implant radiation therapy involving the skeleton.
- Concurrent bisphosphonate and NATPARA use are not recommended
Kindly Let Us Know If This Was helpful? Thank You!


